CAMLOG&Science – Chapter 4
PRE-CLINICAL
STUDIES
Various pre-clinical studies have been performed to evaluate the biological
behavior and reliability of the CAMLOG
®
and CONELOG
®
Implant Systems
in vivo. Design changes and developments to improve the formation and
maintenance of the soft and hard-tissue structures have systematically
been tested in animal studies to prove their state-of-the-art technology.
IMPROVEDOSSEOINTEGRATIONWITH CAMLOG
®
PROMOTE
®
PLUS
DESIGN
The machined surface segment of the CAMLOG
®
SCREW-LINE implant neck
was significantly reduced from 2.0 mm (Promote
®
) to 0.4 mm (Promote
®
plus).
Schwarz et al. (2008) investigated the effect of this design change on crestal
bone resorption in a dog study. Both implant types were inserted in the man-
dibles of dogs following the standard protocol (0.4 mm above the bone crest).
Histological evaluation took place after 2 and 12 weeks. Bone changes were
found in both implant types after 12 weeks. However, the coarse neck area
in the SCREW-LINE Promote
®
plus implants appeared to have a positive effect
on marginal bone growth. Data demonstrated that the new surface design
efficiently reduced crestal bone changes. Another conclusion was that when a
native thick gingiva was available, an approximately 1 mm higher bony in-
tegration level of the implant could be accomplished without the marginal
epithelium reaching the microstructured surface (Becker et al., 2006).
EFFECT OF MICROLEAKAGE ON CRESTAL BONE RESORPTION
Microgaps in the implant-abutment connection have been supposed to play
a critical role in the crestal periimplant bone loss observed during the first
year of loading. Steinebrunner et al. (2005a and b) hypothesized that the
implant-abutment connection may be a reason for the different bacterial
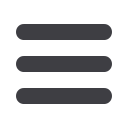
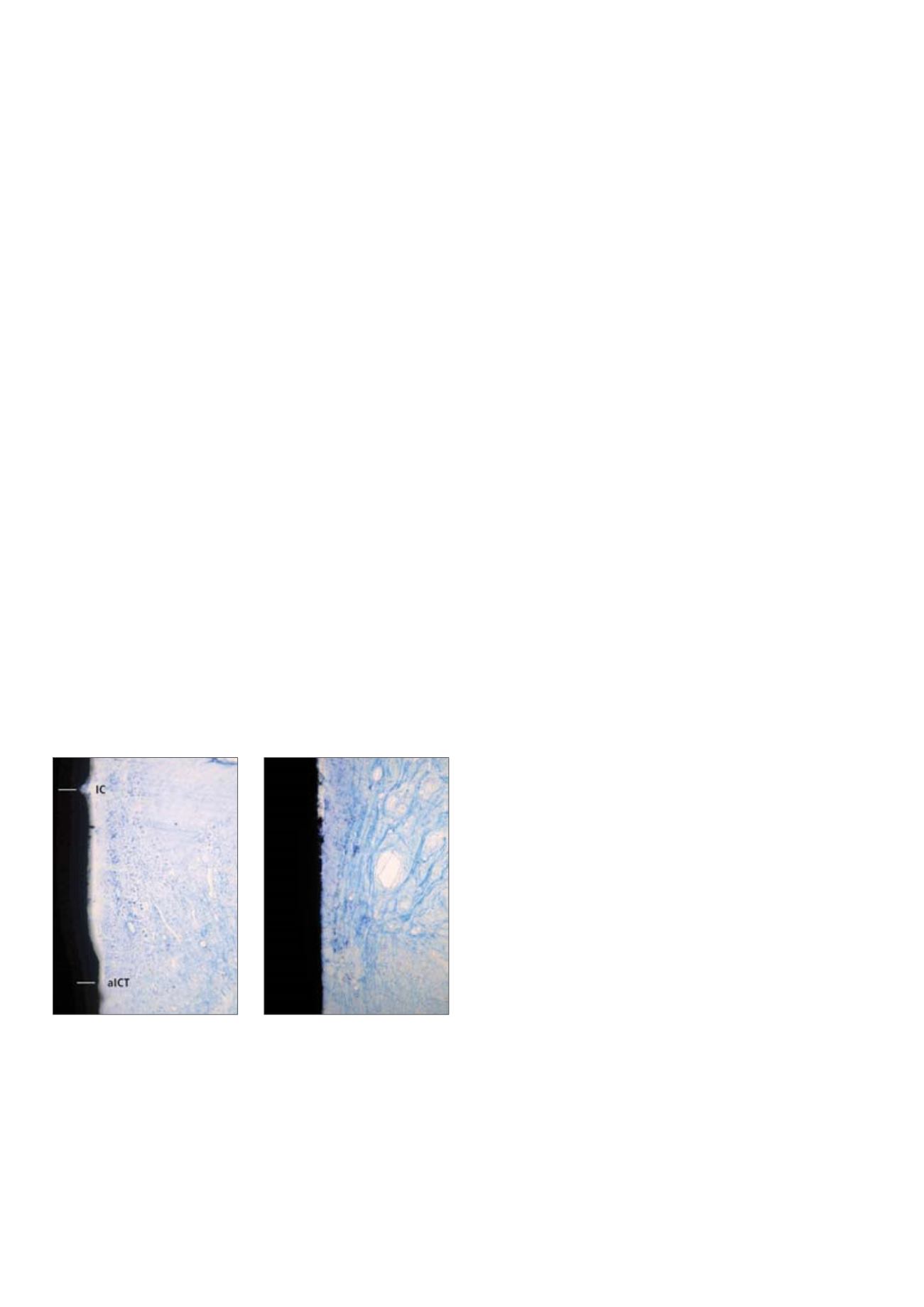
penetration profiles of various implant systems. Schwarz et al. (2008) detected
only a mild inflammatory cell infiltrate at the implant-abutment interface of
both implants, which was divided from the alveolar bone crest by an intact
connective tissue zone (Fig. 14). The authors concluded that microleakage
played no part in marginal bone resorption in the two groups.
CAMLOG K-SERIES: EFFECT OF PLATFORM SWITCHING DESIGN
Platform switching is intended to increase the distance between the im-
plant-abutment interface and the alveolar crest and thereby decrease the
effect of inflammatory cell infiltrates on bone resorption. The principle of
platform switching in the CAMLOG
®
Implant Systemwas evaluated in a dog
study over six months (Becker et al., 2009). SCREW-LINE Promote
®
plus im-
plants (K-series, ø 3.8 mm) were inserted according to the standard surgical
protocol (Fig. 15A: Wide-body matching healing abutments ø 3.8 mm, H 4 mm,
standard configuration) and non-matching abutments (Fig. 15B: ø 3.2 mm,
H 4 mm, platform switching configuration) were connected in a randomized
split-mouth design and served either as control or test implants with a
circumferential horizontal platform of 0.3 mm, respectively. The histological
evaluation after four weeks demonstrated formation of mature woven bone
in the gap between the alveolar bone and the implant surface in both
groups. A first tendency for crestal bone changes was noticed in both
groups. At 12 weeks, mainly mature lamellar bone was found. Bone loss
tended to be slightly increased for the control implants compared to the
platform-switched implants. The difference between control and test im-
plants regarding the distance between implant shoulder and bone crest (IS-BC)
was 0.5 mm at the buccal aspect and 0.4 mm at the lingual aspect (p < 0.05),
respectively. A similar result could be observed at six months when remo-
delling at the alveolar crestal bone seemed to decline (Figs. 15C and 15D).
The difference of IS-BC between both groups was settling down to
approximately 0.3 mm.
The study demonstrated that the CAMLOG
®
implant design (K-Series) both in
its standard and in its platform switching configuration successfully
integrated into hard and soft tissue. Bone remodelling as well as soft-tissue
adaption appeared to beminimal at the implant-abutment interface during the
first eight weeks of osseointegration and considerably less pronounced after
sixmonthsresultinginastablecrestalbonelevel.Theplatform-switchedimplants
tended to yield better results regarding maintenance of the bone level.
Fig. 14:
Histological pictures after 12 weeks healing of (a) Promote
®
and (b) Promote
®
plus
CAMLOG
®
SCREW-LINE implants (200x magnification, toluidine blue stain). The apical extension
of the inflammatory cell infiltrate (aICT) and the level of the alveolar crest are clearly divided
from each other by an intact connective tissue zone with parallel collagen fibers and a few formed
blood vessels; IC = implant shoulder (reproduced from Schwarz et al. 2008; with kind permission
of Quintessence Publishing Co, Inc, USA).
















